Beta-Blocker Overdose — A Practical ED Guide (TOXBASE-Referenced)
Emergency Medicine | MRCEM & FRCEM aligned by Dr. Tajwer Shaheryar | Founder, Golden Hour in ER Golden Hour in ER
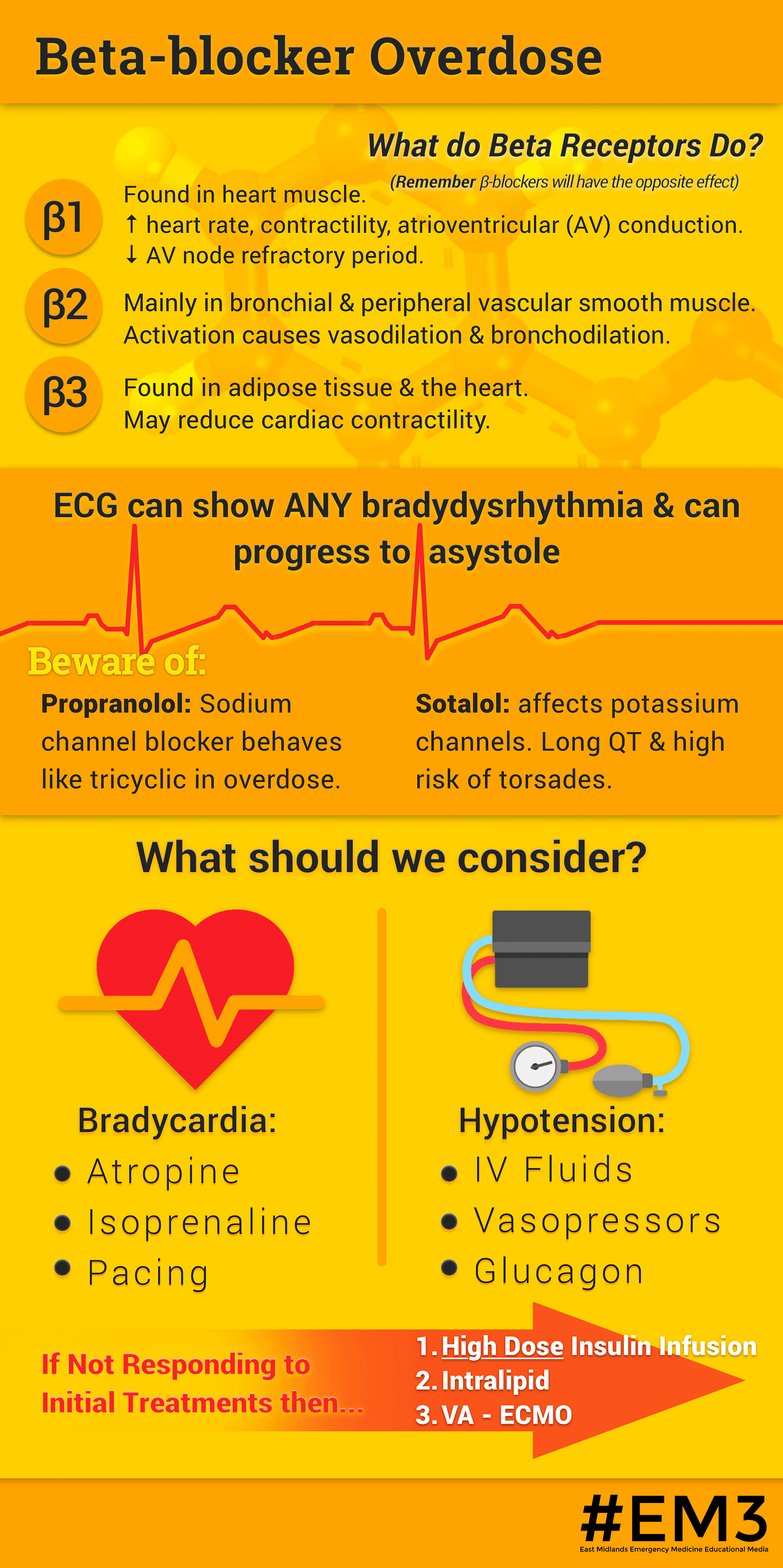
Why Beta-Blocker Overdose Is Dangerous
TOXBASE summary:
β-blockers reduce heart rate, myocardial contractility, and AV nodal conduction. In overdose this may lead to severe bradycardia, hypotension, cardiogenic shock, arrhythmias, seizures, and cardiac arrest.
Key TOXBASE principle:
β1-selectivity is lost in overdose.
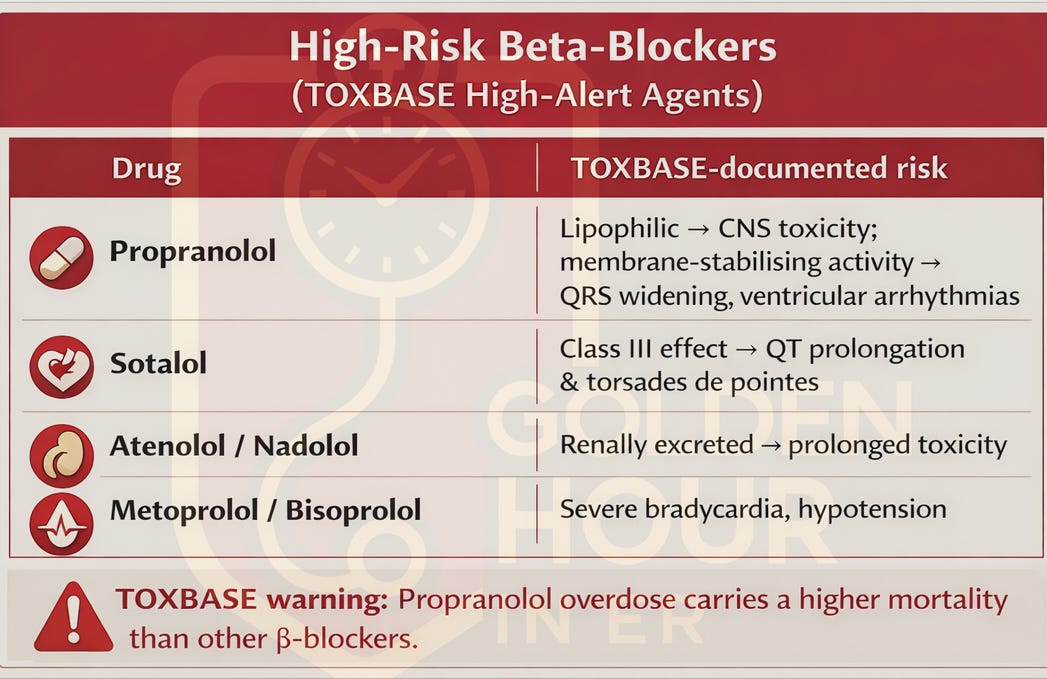
High-Risk Beta-Blockers
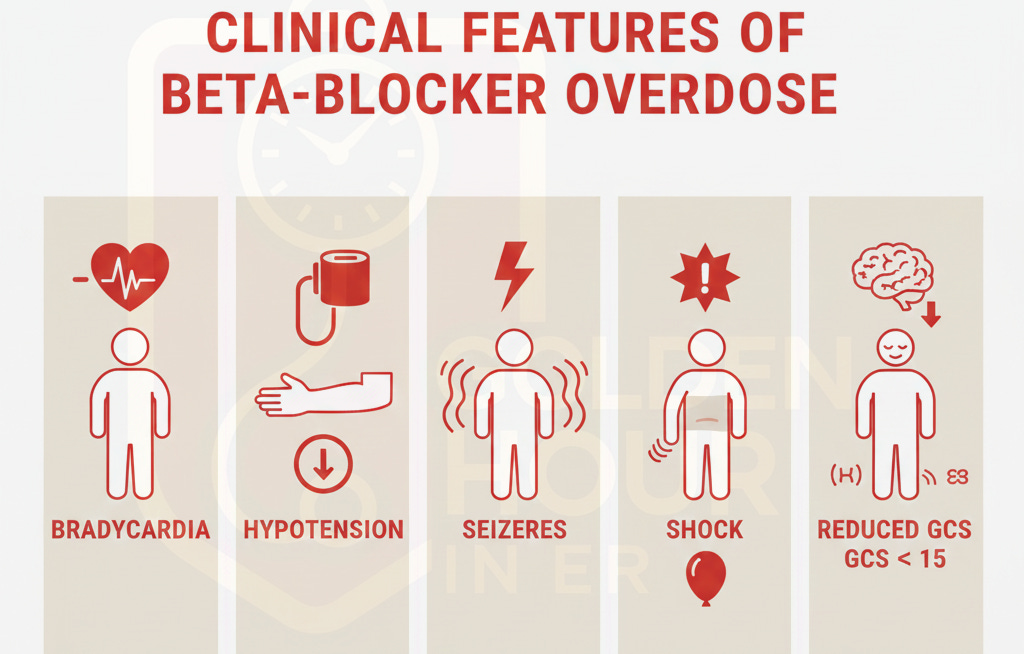
Clinical Features
Cardiovascular
Sinus bradycardia
AV block
Hypotension → shock
Ventricular arrhythmias (MSA drugs)
Neurological
Reduced GCS
Seizures (classically propranolol)
Coma
Metabolic
Hypoglycaemia (especially children)
ECG Findings
Bradycardia
AV conduction delay
Wide QRS (membrane-stabilising activity)
QT prolongation (sotalol)
Initial Management
Airway
Early intubation if ↓GCS or seizures
Anticipate vomiting (glucagon)
Breathing
High-flow oxygen
Ventilatory support as required
Circulation
Continuous cardiac monitoring
IV fluids (often insufficient alone)
Disability
Check capillary glucose
Treat seizures promptly
📞 TOXBASE recommendation:
Contact NPIS early in any symptomatic or significant overdose.
Decontamination (TOXBASE)
Activated charcoal within 1 hour
Consider up to 2 hours for modified-release preparations
Contraindicated if airway not protected
Specific & Definitive Treatments
(All directly referenced from TOXBASE management sections)
1️⃣ Glucagon — First-Line Antidote
Mechanism (TOXBASE):
Increases intracellular cAMP independent of β-receptors → improves heart rate and contractility.
Adult dosing
IV bolus 5–10 mg
Follow with infusion if haemodynamic response observed
⚠️ Adverse effects: vomiting, hyperglycaemia
📌 TOXBASE exam line:
Glucagon is the specific antidote for β-blocker toxicity.
2️⃣ Vasopressors
Adrenaline or noradrenaline
Often required early
TOXBASE notes poor response when used alone
3️⃣ High-Dose Insulin Euglycemic Therapy (HIET)
TOXBASE indication:
Refractory hypotension or shock despite fluids, glucagon, and vasopressors.
Mechanism
Improves myocardial carbohydrate utilisation
Direct positive inotropic effect
Typical adult regimen
Insulin bolus: 1 unit/kg IV
Infusion: 1–10 units/kg/hour
Dextrose infusion to maintain euglycemic
Mandatory monitoring
Blood glucose
Potassium
📌 TOXBASE emphasis: HIET is a key life-saving therapy.
4️⃣ Sodium Bicarbonate
TOXBASE indication
Wide QRS complexes
Ventricular arrhythmias due to membrane-stabilising activity
Especially important in propranolol overdose.
5️⃣ Seizure Control
Benzodiazepines first-line
TOXBASE advises against phenytoin
Advanced / Rescue Therapies (TOXBASE)
Temporary pacing (often ineffective alone)
Intralipid emulsion for severe lipophilic drug toxicity
ECMO for refractory cardiogenic shock (specialist centres)
Observation & Disposition
MRCEM & FRCEM SBA Pearls
Propranolol → seizures + wide QRS
Glucagon = first-line antidote
HIET = definitive escalation
Pacing is unreliable
β-blocker + CCB = very high mortality
Key TOXBASE Memory Line
“Beta-blocker shock doesn’t respond to adrenaline alone — think glucagon, then insulin.”
🔖 TOXBASE Reference List
TOXBASE®, National Poisons Information Service (UK)
Beta-adrenoceptor blocking drugs — overview
Propranolol — toxicity and management
Atenolol / Sotalol — toxicity profiles
High-dose insulin euglycaemic therapy guidance
(Access via www.toxbase.org – subscription required)
About the Author
👨⚕️ Dr. Tajwer Shaheryar
Founder — Golden Hour in ER
Emergency Medicine Physician | MRCEM | Educator💡 Follow for MRCEM exam strategies, RCEM updates & EM insights:
📸 Instagram: @golden.hour.in.er
🎥 YouTube: Golden Hour in ER
📬 If you found this helpful...
Subscribe to Golden Hour in ER on Sub stack for more high-yield EM stories, real exam insights, and upcoming MRCEM OSCE & SBA sessions.
💻 Courses & mentoring: Email at drtj_erdoc@goldenhouriner.com